The “Skinny” on Drinking With Meals & Weight Loss After WLSI have heard many times from new patients to our Program that they have a friend, coworker or family member who has had weight loss surgery and were never told not to drink with their meals. My question is always, “How are they doing with their weight loss?” Although success with weight loss surgery is not achieved with just one behavior modification or diet choice, drinking with meals is a problematic behavior.Not drinking with meals and not drinking for 30 minutes following a meal is one of the best pieces of advice I could provide to a patient to help them lose weight, regardless as to if they have had bariatric surgery or not.
Many of us are familiar with the famous Nathan’s Hot Dog Eating Contest every July 4th in which contestants compete to see how many hot dogs they can eat in a 10-minute period. These contestants not only train for this event, they have a strategy to win it. Although difficult for some of us to watch, you’ll find that that strategy includes soaking the hot dog and bun in liquid to allow for the faster transit of food and better compression of food into the stomach cavity. This is followed by a sip of liquid. Although the issue for postsurgical patients is not about compacting food, or getting food to pass quickly, (we’re talking about a ¾ cup of food not 61 hot dogs), the benefit of not drinking with the meal is two-fold and clearly a great tool for weight loss. Reasons For Not Drinking With Meals - Stay Full Longer! First, by allowing food to sit in the stomach longer, which happens when food is not mixed with liquid, the patient experiences more fullness and the signal is sent to the brain that it’s time to stop eating. Second, when liquid is added to solid food and mixes with stomach acids, the food literally liquefies faster and moves from the stomach down into the intestine at an accelerated rate. With the stomach emptying faster, and the feeling of fullness not being truly experienced, both physical and emotional hunger return more quickly. This begins the cycle of increasing the amount of food the patient is able to eat (physical) as well as the patient’s need to eat more (emotional), sabotaging a patient’s weight loss success. Not drinking with your meals is a good tool for all of us trying to lose weight. One of my patients shared with me that when she was preparing for weight loss surgery, her spouse asked how he could be supportive of her as she moved through the process. Her one and only request to him was that he also not drink with the meals they shared together. Because of their schedules, this generally meant just one meal a day. That said, during the six months of her preparation process, with just this one change at this one meal, he lost 10 pounds! Thankfully, she lost a few more pounds than he did as that might have been a sore subject, but I share this story often to demonstrate the importance of this one behavior change that can truly make a difference when trying to lose weight. |
Appetite Suppressants, Magic or Myth?
Appetite Suppressants, Magic or Myth? On occasion, I am asked about the need or use of appetite suppressants following weight loss surgery. Although a simple question, there are many variables that I would consider before providing an answer.For Gastric Band patients - In broad terms, I am much more inclined to endorse appetite suppressants with post-surgical Gastric Band patients then others, if they are following up for the adjustments and if they are being adherent to the guidelines and behaviors required to be successful with weight loss following gastric banding, (chewing food to applesauce consistency, eating protein forward meals, not drinking with their meals, allowing adequate time for the fullness signal to be experienced, and not grazing or eating without hunger). In these situations, the Gastric Band patient might need a little “jump start” to help them eliminate their feeling of hunger. In these cases, I think appetite suppressants are helpful. For Roux en Y (RNY) or Sleeve patients (I don’t do the Duodenal Switch) - For these patients who are experiencing weight gain, I am much more inclined to look for an answer outside of a medication. I want to make sure that the “tool” is intact and that there is not some breakdown or reversal in place to the operation that allows the patient to regain weight. I will order an upper endoscopy for measurements as well an upper GI swallow exam to better answer this question. If the Bypass or Sleeve is intact, then I want to make sure that the patient is working with the tool and not choosing behaviors to effectively bypass the anatomy such as eating poor food choices, eating without hunger, eating past hunger or grazing throughout the day
Your Relationship With Food Instead of Pills Let me share this experience that happened early in my career as an example. My wife and I were working with a young lady on a personal financial matter. One of the forms requiring our information asked our professions. As our discussion progressed, this woman inquired what type of a surgeon I was, and I told her that I was a general surgeon but 95% of my practice was weight loss surgery. She then shared with me that she had that surgery (RNY) and had gained all of her weight back. I asked what could she eat and she said that she ate “¾ of a pizza” last evening. I was convinced that she had a breakdown of her Gastric Bypass. I encouraged her to get me copies of her records and to make an appointment with me for further evaluation. She came to see me two weeks later. I ordered the upper GI and upper endoscopy. When the results came back, everything was perfect. I saw her back in the clinic the following week to discuss these results. I again asked if she really could eat ¾ of a pizza. When she answered yes, I asked, “Does it hurt?” “Oh, yes” she replied, “I get crushing chest pain up to my throat which lasts for three to four hours.” Now the picture was clear. She was able to eat this large amount by compressing and stacking the pizza up into her esophagus and throat. It was not until the pizza could move through the small Gastric Bypass pouch and be digested that her pain would resolve. For this woman, there is not a pill in the world that will help her to get back on track with weight loss. What was needed was behavioral counseling to relearn how to use the tool she had been given to lose weight. This was a prime and profound example for me of a patient’s need to reevaluate her relationship with food. That said, my standard plan of care for patients that have had either the RNY or Sleeve procedures with concern for weight regain and breakdown of their original procedure, is as follows. First, get an accurate weight history, acquire accurate accounting of their daily calorie/meals, inquire about maladaptive behaviors and evaluate the RNY or sleeve anatomy. In 9 times out of 10, the issue is not anatomical but, if it is, we proceed to revisional surgery to correct the problem. For everyone else, we work on helping the patient get back on track - to relearn the behaviors necessary for successful weight loss following weight loss surgery. Obviously, this is why it is so important for patients to have surgery first and foremost with an experienced surgeon who can perform these operations effectively to appropriately reduce the size of the stomach to allow for significant weight loss. Just as important is that the patient’s care is with a comprehensive bariatric program to ensure that they have the expertise and the support they might need if they do begin to struggle with weight regain. I have seen some crazy foreign operations for “WEIGHT LOSS”. What Is Your Best Approach? Weight loss, for Band patients, may involve appetite suppressants, but for most others, most likely will involve emotional support to get them back on track for weight loss. If indicated following RNY or Sleeve, a bariatrician would best direct this part of your journey into health.
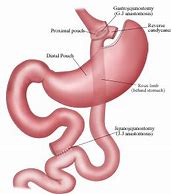
The Roux-en-Y Gastric Bypass is a surgical operation that causes weight loss by both limiting the amount of food that a person is able to eat (restrictive) while causing malabsorption of the nutrition and calories consumed. The intestinal Roux limb of the Roux en Y is re-attached much lower in the intestinal tract, causing less intestinal length for absorption. The question I have been asked by the ObesityHelp.com Community is, “Does malabsorption of the Roux-en-Y Gastric Bypass pouch change over time?” This is a question that we likely will never be able to directly measure, but it might. This is why I say it might.
Let’s begin with three different patient examples.
Malabsorption with the Gastric Bypass Patient 1
My first patient is “FP”, a 55-year-old male who came to my office interested in weight loss surgery because he was morbidly obese. FP and I sat down and began reviewing his health history. This was early in my career and before gastric banding surgery or Endoluminal procedures (such as Gastric Balloons), so we were discussing the possibility of FP having the gastric bypass operation.
In reviewing FP's history, he shared that he had been in a near-fatal car accident when he was 16 years old. He sustained serious abdominal injuries. He underwent life-saving surgery which required removal of almost all of his small intestine. The accident was so severe and his intestinal loss so profound that, following the accident, he was not able to consume and absorb enough calories to sustain life.
FP existed on TPN (nutrition through an IV). FP required TPN for the next five years, while slowly transitioning back to a normal diet. His intestine did not grow in length, but it did adapt by increasing its ability to absorb. This continued to today where he is now absorbing so many calories that he is morbidly obese. Obviously, he was not a candidate for the Gastric Bypass operation since he has so very little small intestine, but his story of intestinal recovery amazed me.
Malabsorption with the Gastric Bypass Patient 2
My second patient is “SP” and she underwent a Roux-en-Y gastric bypass in 2008, only to be readmitted several days following surgery with severe abdominal pain. She was taken back into surgery for an emergent abdominal exploration, which demonstrated almost all of her small intestine had lost blood flow due to an undiagnosed and unknown complication of a blood clotting disorder. She was seriously ill and was in the Intensive Care Unit for several months. SP underwent several operations in attempts to save her small intestine which were, for the most part, unsuccessful. There were even discussions about a possible intestinal transplant. All but 100 cm of her intestine had to be ultimately removed.
As with FP, SP’s life was sustained by IV nutrition for the next two years. She slowly transitioned back onto a regular diet. In monitoring her nutritional needs, when she started eating regular food, she demonstrated severe malabsorption with the inability to absorb fluids, critical vitamins and/or nutrients. Over the next 10 years her small intestine, though limited in length, was able to adapt and increase its ability to absorb. Today she is in an almost normal state of health.
In SP’s case, she is not morbidly obese, and actually maintains a healthy weight, so there is that difference. Also, she is 10 years out from surgery while FP is 35 years out. Again, I do not know if this makes a difference.
What I do believe is that each of us adapts to challenges differently but because of my own experience with FP and with SP, I believe that intestinal malabsorption for whatever reason can progress and improve over time.
If Malabsorption is Less, What’s the Difference for Roux en Y Weight Loss of Long Limb versus Short Limb Procedures?
Malabsorption: In an excellent study, researchers took individuals whose BMI averaged 50 or above and randomized them into one of two groups. The only difference, the first group had a very short intestinal Roux limb (less malabsorption), the second group had a very long intestinal Roux limb (more malabsorption).
The thought was that the patients with the longer intestinal Roux limb and more intestinal malabsorption should lose more weight. What they found to be true is that the percentage of weight loss was exactly the same for each group. The longer limb, with more malabsorption, did not allow for more weight loss. The only difference found was the group with the longer Roux limb and more malabsorption had more nutritional deficiencies.
With this in mind, I personally make very small Sleeve stomachs. The Sleeve stomach has a normal inlet and normal outlet and normal digestion so there is no malabsorption.
If you compare my Sleeve patients’ excess weight loss to my Roux-en-Y patients’ excess weight loss, here are the numbers.
So, with these two comparisons in mind, one might argue that:
This takes me to a final story and my final patient. Several years ago, my wife and I were refinancing our home and we met with our broker to finalize all of our paperwork. As we began signing the multitudes of papers required for this process, we began to chat. She asked me what I did and I told her that I was a bariatric surgeon. She got very excited and stated she had that operation but she has gained all of her weight back. I was surprised. We began talking about what food choices she was making and the quantity of food that she could eat. “Well,” she answered,“last night I ate ¾ of a pizza.” With this, I told her I thought her bypass must have broken down, and I asked her to get her medical records and to make an appointment to see me to see if I could help. Her records arrived prior to our visit, and I reviewed her operation report, which described a very standard Roux-en-Y operation. I saw her in my clinic and ordered several studies to best evaluate her gastric bypass anatomy. I reviewed those test results which defined a perfect, intact gastric bypass. After discussing these normal findings with her, I again asked if she really could eat ¾ of a pizza. She said she definitively could. Baffled, I then asked if it hurt after she had done this. “Oh yes,” she responded, "I get crushing chest pain up to my throat that lasts for hours.” What became apparent was that my broker was able to ¾ of a pizza because she was stacking the pizza in her esophagus up to her throat. This caused her intense pain lasting for hours, or about the time it takes for the pizza to move down into normal digestion. There was nothing that I could do surgically to improve or correct her operation. What needed to change was her relationship to food. I scheduled her to meet with our nurse clinician, our psychologist, and our dietician to help her to get back on track with her weight loss tool.
With all this in mind, if you are a patient a few years out following Roux en Y gastric bypass and are finding yourself regaining weight, a change in your bypass malabsorption would not be my first consideration causing that weight gain. I would recommend, as I do in my practice, to reconnect with the dietician in your program – review your food choices and portion size, and determine together if there is an underlying issue or if you really just need to get back on track with diet choices and exercise. In my experience, nine times out of ten, this is the case.
My answer to the question asked? I do believe that there can be a change in malabsorption following the Roux-en-Y gastric bypass with some patients, and this change might allow for more food tolerances. Could these food tolerances cause weight regain? Possibly, but I do not believe that having less malabsorption alone, would be significant enough to be the single cause of substantial weight regain.
And...on final note, take all of our required vitamins and supplements every day to maintain optimal health!
In closing, I would like to address a very important consideration following the gastric bypass operation and its inherent malabsorption. Because of the malabsorptive component with this procedure, it is imperative for any patient having had Roux en Y gastric bypass surgery, to take all of their required vitamins and supplements every day for the rest of their life. In our program, these vitamins include a complete multivitamin, Calcium, Vitamin D, B12, and possibly iron. Otherwise, you are at risk for vitamin and mineral deficiencies that could lead to long-term health issues - it is why an annual assessment of your nutritional fitness is so important. In our program, this analysis includes evaluating your parathyroid activity (intact PTH), vitamin D level, B vitamin support (thiamine, B12, and folate), Hgb, iron stores, protein support (albumin) as well possibly zinc, copper, and/or other fat-soluble vitamin levels if indicated. Annual labs allow you to be assessed, and your supplementation altered, if needed, to maintain you in optimal health.
Let’s begin with three different patient examples.
Malabsorption with the Gastric Bypass Patient 1
My first patient is “FP”, a 55-year-old male who came to my office interested in weight loss surgery because he was morbidly obese. FP and I sat down and began reviewing his health history. This was early in my career and before gastric banding surgery or Endoluminal procedures (such as Gastric Balloons), so we were discussing the possibility of FP having the gastric bypass operation.
In reviewing FP's history, he shared that he had been in a near-fatal car accident when he was 16 years old. He sustained serious abdominal injuries. He underwent life-saving surgery which required removal of almost all of his small intestine. The accident was so severe and his intestinal loss so profound that, following the accident, he was not able to consume and absorb enough calories to sustain life.
FP existed on TPN (nutrition through an IV). FP required TPN for the next five years, while slowly transitioning back to a normal diet. His intestine did not grow in length, but it did adapt by increasing its ability to absorb. This continued to today where he is now absorbing so many calories that he is morbidly obese. Obviously, he was not a candidate for the Gastric Bypass operation since he has so very little small intestine, but his story of intestinal recovery amazed me.
Malabsorption with the Gastric Bypass Patient 2
My second patient is “SP” and she underwent a Roux-en-Y gastric bypass in 2008, only to be readmitted several days following surgery with severe abdominal pain. She was taken back into surgery for an emergent abdominal exploration, which demonstrated almost all of her small intestine had lost blood flow due to an undiagnosed and unknown complication of a blood clotting disorder. She was seriously ill and was in the Intensive Care Unit for several months. SP underwent several operations in attempts to save her small intestine which were, for the most part, unsuccessful. There were even discussions about a possible intestinal transplant. All but 100 cm of her intestine had to be ultimately removed.
As with FP, SP’s life was sustained by IV nutrition for the next two years. She slowly transitioned back onto a regular diet. In monitoring her nutritional needs, when she started eating regular food, she demonstrated severe malabsorption with the inability to absorb fluids, critical vitamins and/or nutrients. Over the next 10 years her small intestine, though limited in length, was able to adapt and increase its ability to absorb. Today she is in an almost normal state of health.
In SP’s case, she is not morbidly obese, and actually maintains a healthy weight, so there is that difference. Also, she is 10 years out from surgery while FP is 35 years out. Again, I do not know if this makes a difference.
What I do believe is that each of us adapts to challenges differently but because of my own experience with FP and with SP, I believe that intestinal malabsorption for whatever reason can progress and improve over time.
If Malabsorption is Less, What’s the Difference for Roux en Y Weight Loss of Long Limb versus Short Limb Procedures?
Malabsorption: In an excellent study, researchers took individuals whose BMI averaged 50 or above and randomized them into one of two groups. The only difference, the first group had a very short intestinal Roux limb (less malabsorption), the second group had a very long intestinal Roux limb (more malabsorption).
The thought was that the patients with the longer intestinal Roux limb and more intestinal malabsorption should lose more weight. What they found to be true is that the percentage of weight loss was exactly the same for each group. The longer limb, with more malabsorption, did not allow for more weight loss. The only difference found was the group with the longer Roux limb and more malabsorption had more nutritional deficiencies.
With this in mind, I personally make very small Sleeve stomachs. The Sleeve stomach has a normal inlet and normal outlet and normal digestion so there is no malabsorption.
If you compare my Sleeve patients’ excess weight loss to my Roux-en-Y patients’ excess weight loss, here are the numbers.
- My Sleeve patients are typically restricted to a ¾ cup to 1 cup of food, and on average lose 68% excess weight in one year.
- My Roux-en-Y patients are restricted to a ¾ to 1 cup of food, and on average lose 73% excess weight in one year.
So, with these two comparisons in mind, one might argue that:
- The malabsorption component of the Roux En Y contributes to a smaller percentage of the total amount of weight loss that follows Roux en Y surgery and;
- The amount or degree of malabsorption has little or no effect on total excess weight loss which, in the cases from the above research study, demonstrated that more malabsorption is not better.
This takes me to a final story and my final patient. Several years ago, my wife and I were refinancing our home and we met with our broker to finalize all of our paperwork. As we began signing the multitudes of papers required for this process, we began to chat. She asked me what I did and I told her that I was a bariatric surgeon. She got very excited and stated she had that operation but she has gained all of her weight back. I was surprised. We began talking about what food choices she was making and the quantity of food that she could eat. “Well,” she answered,“last night I ate ¾ of a pizza.” With this, I told her I thought her bypass must have broken down, and I asked her to get her medical records and to make an appointment to see me to see if I could help. Her records arrived prior to our visit, and I reviewed her operation report, which described a very standard Roux-en-Y operation. I saw her in my clinic and ordered several studies to best evaluate her gastric bypass anatomy. I reviewed those test results which defined a perfect, intact gastric bypass. After discussing these normal findings with her, I again asked if she really could eat ¾ of a pizza. She said she definitively could. Baffled, I then asked if it hurt after she had done this. “Oh yes,” she responded, "I get crushing chest pain up to my throat that lasts for hours.” What became apparent was that my broker was able to ¾ of a pizza because she was stacking the pizza in her esophagus up to her throat. This caused her intense pain lasting for hours, or about the time it takes for the pizza to move down into normal digestion. There was nothing that I could do surgically to improve or correct her operation. What needed to change was her relationship to food. I scheduled her to meet with our nurse clinician, our psychologist, and our dietician to help her to get back on track with her weight loss tool.
With all this in mind, if you are a patient a few years out following Roux en Y gastric bypass and are finding yourself regaining weight, a change in your bypass malabsorption would not be my first consideration causing that weight gain. I would recommend, as I do in my practice, to reconnect with the dietician in your program – review your food choices and portion size, and determine together if there is an underlying issue or if you really just need to get back on track with diet choices and exercise. In my experience, nine times out of ten, this is the case.
My answer to the question asked? I do believe that there can be a change in malabsorption following the Roux-en-Y gastric bypass with some patients, and this change might allow for more food tolerances. Could these food tolerances cause weight regain? Possibly, but I do not believe that having less malabsorption alone, would be significant enough to be the single cause of substantial weight regain.
And...on final note, take all of our required vitamins and supplements every day to maintain optimal health!
In closing, I would like to address a very important consideration following the gastric bypass operation and its inherent malabsorption. Because of the malabsorptive component with this procedure, it is imperative for any patient having had Roux en Y gastric bypass surgery, to take all of their required vitamins and supplements every day for the rest of their life. In our program, these vitamins include a complete multivitamin, Calcium, Vitamin D, B12, and possibly iron. Otherwise, you are at risk for vitamin and mineral deficiencies that could lead to long-term health issues - it is why an annual assessment of your nutritional fitness is so important. In our program, this analysis includes evaluating your parathyroid activity (intact PTH), vitamin D level, B vitamin support (thiamine, B12, and folate), Hgb, iron stores, protein support (albumin) as well possibly zinc, copper, and/or other fat-soluble vitamin levels if indicated. Annual labs allow you to be assessed, and your supplementation altered, if needed, to maintain you in optimal health.
Revision Following Gastric Bypass: Are You a Candidate and What are Your Options?
If you are reading this article, most likely you are a patient who has had previous gastric bypass surgery and, more than likely did well following the initial surgery but now may have regained some of your initial weight loss. The definition of success following weight loss surgery is losing 50% or more of your excess weight (ie: If you were 100 pounds overweight, you would lose 50 pounds) and keeping that weight off for greater than 5 years. If you have regained weight following gastric bypass surgery and are just trying to figure out the "why" of that regain, it is important to consider all potential causes.
For most patients, in the first year following surgery, the weight loss experience seems nothing short of remarkable. They are feeling good, getting kudos from family, friends and coworkers and existing on a personal high of positive emotion. It is much easier, at this point to stay on task with diet and exercise because there is such support to do so. But what happens when weight loss slows or stops? Fast forward a few years... it is not uncommon for patients at years 3-5 following surgery, to become a little more lax with their diet and maybe not so adherent to a solid work out routine. In our Program, we encourage all of our patients see both the surgeon as well as the dietician at every annual visit. This is to allow us to touch base with every patient to best support their overall health and weight loss efforts and to identify any potential pitfalls that might impede their continued weight loss. Our exercise physiologist is also available for anyone preoperatively and postoperatively to help those who have gotten away from their exercise routine and to help to get a jump start on physical activity. Sometimes it is really just working with the patient to get them re-energized and focused on their healthy goals that is needed. If, however, in addition to weight regain, you have other symptoms too, such as abdominal pain, dumping or other intestinal dysfunction, then a more comprehensive work up is in order.
Where do we start? First, I would recommend that you undergo a barium swallow study which, in simple terms, is a radiology test in which the patient drinks a small amount of special colored dye and, under x-ray, the radiologist watches that dye as it moves through the digestive tract. This diagnostic helps to identify if there is an enlarged pouch, or if the opening between your stomach and small intestines (the stoma) has stretched and is too large. If either an enlarged pouch or a dilation stoma are found, the next diagnostic study, and one which I perform with all of my patients so I am able to personally observe the result, is an EGD or upper endoscopy. With mild sedation, a tube and camera is placed through the patients mouth and down their esophagus into the stomach for further assessment of the stomach and stoma. At that time, other areas of the anatomy including staple line, esophageal abnormalities, roux limb abnormalities and the gastrogastric fistula can also be assessed. If there is an anatomic abnormality, then surgery may be indicated. What are your options if this is the case. In my practice, you have three surgical options. These are: 1. Transoral Outlet Reduction (TORe), 2. Banding over Bypass, 3. Revision of Candy Cane Deformity. Let's take a look at each of these individually.
Transoral Outlet Reduction (TORe): This is an endoscopic procedure which is the least invasive procedure of all of the revisional options. In this procedure, using an endoscope (so again inserting a tube and camera through the mouth and down the esophagus and into the stomach, I suture the stomal opening to a much smaller size as well suture the pouch to reduce pouch size. This allows for faster fullness with reduced stomach size as well longer satiety as food stays in the stomach longer with the reduces stomal opening, allowing the brain to register fullness earlier and for a longer period of time. Many insurance carriers are refusing to cover this procedure with the argument that this is experimental, so often this is a self pay procedure for patients and rages from $8,000 to $10,000. The procedure is performed on an outpatient basis and patients are back to normal within 48 hours.
Band over Bypass: This is an inpatient procedure in which a gastric band is placed just the stomal opening. A port component is attached to the abdominal wall. Six weeks following surgery, you will return to the clinic and the band will be adjusted by injecting saline through the port and into the banding device, which will restrict the band down. This is similar in effect to the TORe procedure as it restricts the size of the stomach and the ability for food to pass quickly from the stomach into the intestines. Although a more invasive procedure than the TORe as it is laparoscopic surgery, not endoscopic surgery, most insurance carriers do recognize the banding procedure as a billable code and are more likely to provide coverage for the procedure. If the patient's symptoms are not related to stomal dilation or enlarged pouch, then a candy cane deformity should be considered.
Candy Cane Deformity/Revision: What is a candy cane deformity? Although not common following gastric bypass, some patients do develop a candy cane deformity following Roux en Y gastric bypass surgery. Essentially, part of the small intestines stops functioning, which leads to symptoms such as abdominal pain, nausea and vomiting. Patients with this deformity are also susceptible to weight regain as they often turn to often more to soft, more carbohydrate and higher caloric food choices for easier digestion. This abnormality is easily corrected with a laparoscopic revision in which the non-functioning part of the intestine is removed which leads to, in most cases, resolution of all symptoms. This procedure is generally performed as an inpatient procedure.
If you find yourself with weight regain or any other symptoms such as nausea, pain and vomiting, there is help. I encourage you to get back on track with a comprehensive bariatric center with surgeons that have experience in revisional bariatric surgeries who can work with you to develop a plan to get you back on track, whether that be just with diet and exercise or if there is an anatomical issue that needs surgical intervention. There is an option for you to help you to feel better and to help you to lose weight and move into further into health.